Felty's Syndrome with Nodular Regenerative Hyperplasia of Liver and Portal Hypertension
Sham Santhanam
Sham Santhanam*
Department of Rheumatology, Global Hospitals, Chennai, India
- *Corresponding Author:
- Sham Santhanam
Department of Rheumatology, Global Hospitals
Chennai, India
Tel: 044 2277 7000
E-mail: itsdrsham@gmail.com
Received date: August 13, 2015; Accepted date: October 06, 2015; Published date: October 20, 2015
Citation: Santhanam S. Felty’s Syndrome with Nodular Regenerative Hyperplasia of Liver and Portal Hypertension. J Autoimmun Disod. 2015, 1:1. DOI: 10.21767/2471-8513.100001
Copyright: © 2015 Sham Santhanam. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case report
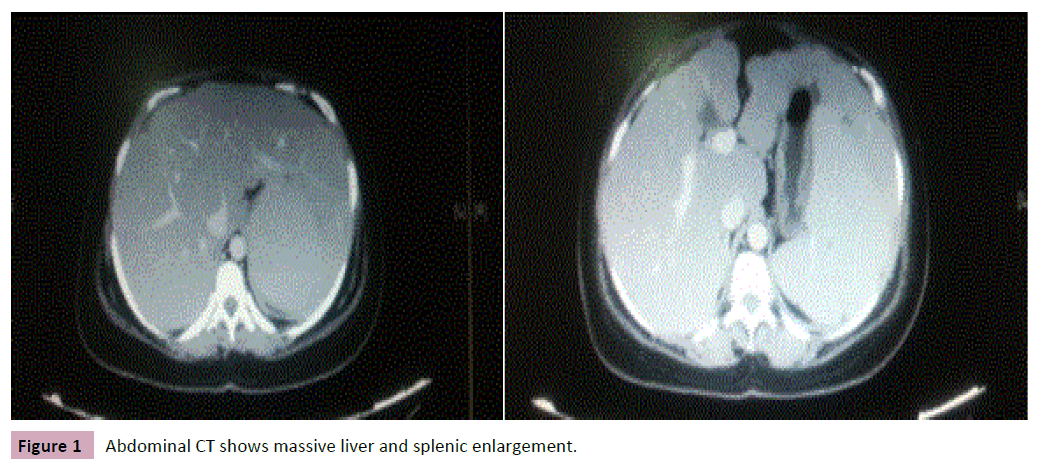
A 32 year old female presented with easy fatigability and breathlessness on exertion of 1 year duration. She also gave history of multiple joint pain and swelling with prolonged early morning stiffness. She complained of diffuse abdominal pain with early satiety and recurrent episodes of fever. She is a known case of hypothyroid on thyroxin supplementation. On examination she was very pale, febrile with multiple furuncles over her labial region with active polyarthritis (involving both small and large joints of upper and lower limbs). On evaluation her Haemoglobin was 4.8 g/dl, total leukocyte counts of 1700 cells/cu.mm (neutrophils–21%) and platelets 75,000 cells/ cu.mm. Her previous investigations showed a gradual decline in counts of all three lineages. Peripheral smear was suggestive of haemolytic anaemia. Her liver function tests were normal except for mild elevation in indirect bilirubin. She had raised Lactate dehydrogenase (LDH) levels with normal renal function and urine examination. Her erythrocyte sedimentation rate (ESR) was 103 mm/hr and C- reactive protein (CRP) of 22.2 mg/dl. She tested positive for Rheumatoid factor (1:640 titre by latex agglutination) and also strongly positive for Anti CCP (cyclic citrulinated peptide) (5.6 by ELISA). All other immunological workup including antinuclear antibody were negative. Bone marrow examination was done which was suggestive of reactive marrow with myeloid hyperplasia and no evidence of malignancy. Her Ultrasonography of abdomen was done, which showed hepatosplenomegaly with an enlarged portal vein (diameter of 16 mm). Computed tomography of abdomen confirmed the same, with enlarged nodular liver and a massive spleen of 21 cm. Her upper GI scopy was normal with no varices. Patient was not willing for a liver biopsy. Her X rays of hand and foot were normal except for soft tissue swelling and juxtraarticular osteoporosis. So a diagnosis of Seropositive Rheumatoid arthritis (RA) with Felty’s syndrome was made. The points to ponder in this case are the presence of portal hypertension, hypersplenism, nodular liver enlargement and relatively short duration of joint symptoms with no joint erosions or deformity.
The patient was initially treated with antibiotics, blood transfusion, G-CSF (Granulocyte – colony stimulating factor) injections followed by steroids (20 mg/day initially and tapered gradually), 400 mg of hydroxychloroquine and 1 g of sulfasalazine. With treatment the patient improved symptomatically (decreased joint pain and swelling) and after 6 months of treatment her blood counts improved with a Haemoglobin of 10 g/dl, total counts of 5600 cells/cu.mm and platelets of 106,000 cells/cu.mm. Her spleen size reduced to 17 cm, portal vein size became normal with reduction in nodularity of liver after 8 months of treatment with above drugs.
Discussion
Felty’s syndrome is one of the rare extra articular manifestations of rheumatoid arthritis described as early as 1924 [1]. But it is rarely seen these days due to early initiation of treatment for rheumatoid arthritis. It comprises the classical triad of joint symptoms (RA) with neutropenia and splenomegaly. Usually it is found in patients with long standing rheumatoid arthritis with joint erosions, deformities and rheumatoid nodules. They usually have HLA DR4 positivity with high titers of rheumatoid factor [2]. But our patient had relatively short duration of disease with no erosions, deformities or rheumatoid nodules. Felty’s syndrome as the presenting manifestation of Rheumatoid arthritis has been rarely reported in literature [2]. Our patient though had joint symptoms previously, she presented only because of worsening of symptoms due to severe anemia. These patients can have commonly skin, soft tissue and upper and lower respiratory tract infections. Our patient had recurrent episodes of fever with soft tissue infections (Figure 1).
Liver involvement in Felty’s syndrome is quite rare but can have an enlarged liver due to ‘Nodular regenerative hyperplasia’. In 1953, Ranstorm first described an entity called as ‘Miliary hepatocellular adenomatosis’ which is now termed as ‘nodular regenerative hyperplasia’ (NRH). It comprises of portal hypertension, liver cell hyperplasia, secondary nodules with minimal or absent fibrosis [4]. In our patient, there was nodular enlargement of liver in both Ultrasound and computed tomography of abdomen. Ideally liver biopsy should be done but a diagnosis of nodular regenerative hyperplasia was assumed, as our patient had a clinical picture of rheumatoid arthritis with massive splenomegaly, pancytopenia, portal hypertension and with other potential causes being ruled out.3 NRH can also be associated with other rheumatological disorders like systemic lupus erythematous, scleroderma, polyarteritis nodosa, antiphospholipid antibody syndrome etc. [3]. Several possible reasons were proposed, like regenerative nodules pressing on intrahepatic blood vessels, obliterative portal venopathy, vasculitis, immune complex deposition etc. [5].
Splenomegaly can be found in 5–10% of RA patients. The causes vary from non-specific hyperplasia of spleen (common) to amyloidosis and rarely Felty’s syndrome [6]. Development of portal hypertension in Felty’s syndrome is rare and having a variceal bleeding is even more rare [7]. Usually the varices due to portal hypertension in Felty’s syndrome get decompressed after splenectomy unlike varices in cirrhotic patients. The other major difference is, patients with a variceal bleed in Felty’s syndrome don’t develop hepatic encephalopathy [5].
There is not much of evidence for management of Felty’s syndrome as its incidence is very rare. All the synthetic disease modifying agents like methotrexate, lefluonomide, sulfasalazine and hydroxycholoroquine has been tried with good response. Among biological agents, there are reports on rituximab being effective in Felty’s syndrome [8]. Our patient had pancytopenia due to hypersplenism and hence initially she was treated with tapering dose of steroids, antibiotics and with G-CSF and blood transfusion. Once her haemoglobin and counts improved, she was started on hydroxychloroquine, sulfasalazine and after 6 months of treatment her blood counts improved and joint symptoms were controlled.
Conclusion
In conclusion, Felty’s syndrome need not always be a long term complication and can occur early without joint erosions or deformity. Rarer features like Nodular regenerative hyperplasia leading to portal hypertension and hypersplenism responds to disease modifying agents and patients respond well to treatment.
References
- Felty AR (1924) Chronic arthritis in the adult associated with splenomegaly and leucopenia: a report of five cases of an unusual clinical syndrome. Johns Hopkins Hosp Bull 35: 16.
- Chavalitdhamrong D, Molovic-Kokovic A, IlievA (2009) Felty's Syndrome as an initial presentation of Rheumatoid Arthritis: a case report. Cases Journal 2:206.
- Bedoya ME, Ceccato F, Paira S (2015) Spleen and Liver Enlargement in a Patient with Rheumatoid Arthritis. Reumatol Clin 11:227-231
- Ranstrom S (1953) Miliary hepatocellular adenomatosis. Acta Pathol Microbiol Scand 33:225-229.
- Stock H, Kadry Z, Jill P, Smith JP (2009). Surgical management of portal hypertension in Felty’s syndrome: A case reportand literature review. Journal of Hepatology 50: 831-835.
- Blendis LM, Ansell ID, Jones KL, Hamilton E, Williams R (1970) Liver in Felty’s syndrome. Br Med J 1:131-135.
- Reisman T, Levi JU, Zeppa R, Clark R, Morton R, et al.(1977) Non cirrhotic portal hypertension in felty’s syndrome. Am J Dig Dis 22:145-148.
- Chandra PA, Margulis Y, Schiff C (2008) Rituximab is useful in the treatment of Felty's syndrome. Am J Ther 15: 321-322.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences