Lethal and Total Lyell Syndrome Induced by Quinine in a Cameroonian Child
Francky Teddy Endomba, Jan Rene Nkeck* and Aude Laetitia Ndoadoumgue
Francky Teddy Endomba1, Jan René Nkeck1* and Aude Laetitia Ndoadoumgue2
1Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Yaoundé, Cameroon
2School of Health and Related Research, The University of Sheffield, United Kingdom
- *Corresponding Author:
- Nkeck Jan René
Faculty of Medicine and Biomedical Sciences
University of Yaoundé I, Yaoundé, Cameroon
Tel: +237696136647
E-mail: jrnkeck@gmail.com
Received date: October 6, 2017; Accepted date: October 16, 2017; Published date: October 18, 2017
Citation: Endomba FT, Nkech JR, Ndoadoumgue AL (2017) Lethal and Total Lyell Syndrome Induced by Quinine in a Cameroonian Child. J Autoimmune Disord 3:45.
Copyright: © 2017 Endomba FT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
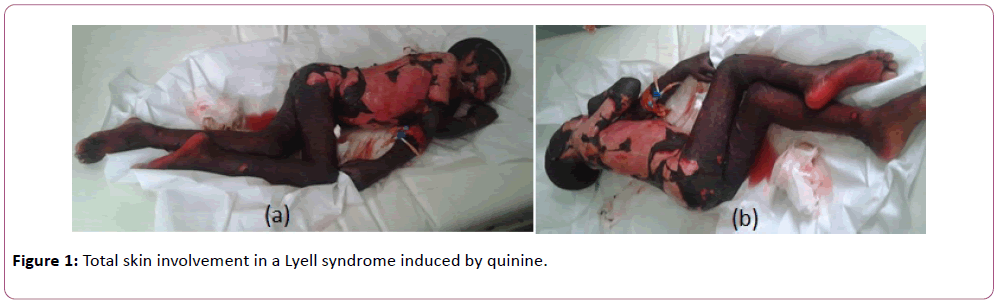
A six years old girl, who presented 3 days’ mild pruritus following oral intake of quinine one year earlier and treated with oral chlorepheniramine, was referred from a tertiary center for an extensive epidermal necrolysis. Five days prior to her consultation, she was treated for malaria with oral quinine (250 mg/8 h) and paracetamol (500 mg/12 h) with good clinical evolution but presented 48 h later with oral squamous lesions and bullous rash. She was brought to the hospital where she received IV ceftriaxone (50 mg/kg/day), gentamicine (3 mg/kg/ day) and dexamethasone (0.15 mg/kg/6 h) meanwhile oral flucloxacilline and quinine was stopped. Due to extension of skin involvement, the child was transferred to the intensive care unit two days after her admission in the hospital. On admission, she was conscious, ill-looking, had low grade fever (38.7°C) and tachypnea (24 cycles/min). She had a 100% cutaneous involvement which included disseminated flaccid bullae, irregularly shaped erythematous macules, large areas of epidermal detachment, and Nikolsky sign (Figure 1).
Mucosal lesions included the lips and eyes (conjunctivitis and eyelid edema). The diagnosis of Lyell syndrome with total involvement of the skin was made. The identified cause was oral quinine according to ALDEN’s (Algorithm of Drug causality for epidermal Necrolysis) criteria and Naranjo’s scores of 4 and 5 respectively. Biological investigations revealed moderate anemia (9 g/dl), mild hyponatremia (132 mmol/l) without any other abnormalities. After prompt withdrawal of all previous drugs, the child was rehydrated with IV normal saline, she received oxygen therapy, wounds care, type I antihistaminic drug, tramadol and ranitidine, all given intravenously. Her state unfortunately worsened progressively and she died after six days in the intensive care unit.
Widely used in sub-Saharan Africa, anti-malarial drugs such as quinine could possibly induce severe adverse cutaneous reactions as Lyell syndrome [1]. The prescription of these medications should be preceded by good questioning focused on adverse manifestations to avoid serious complications. The etiology is mostly estimated through imputability elements [2]. Severe adverse manifestations after taking antimalarial drugs should be reported and the patient quickly and adequately followed up in a specialized unit.
Acknowledgement
We would like to thank Dr Alexandra Elanga, M.D for his collaboration in this work.
References
- Kourouma S, Sangaré A, Kagola M, Kouassi I, Ecra E, et al. (2014) Syndrome de Steven-Johnson et de Lyell : étude de 185 cas au CHU de Treichville (Abidjan, Côte d’Ivoire). Med Sante Trop 24: 94-98.
- Piérard GE, Jennes S, Piérard-Franchimont C (2016) Toxic epidermal necrolysis (Lyell syndrome), a lifethreatening emergency of introgenic origin. Rev Med Liege 71: 435-439.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences