A Unique Case of Crossover Second Toe Syndrome Treated by Autologous Peripheral Blood Stem Cells
Ciro Gargiulo, Van H Pham, Kieu CD Nguyen, Trieu LH Vo, Thao H Duy, Kenji Abe, Mark J Holterman, Melvin Shiffman and Luis Filgueira
Ciro Gargiulo1*, Van H Pham2, Kieu CD Nguyen1, Trieu LH Vo1, Thao H Duy3, Kenji Abe4, Mark J Holterman5, Melvin Shiffman6 and Luis Filgueira7
1Human International Medical Center, Tan Tao University, Ho Chi Minh City, Vietnam
2Nam Khoa Bioteck Ltd/Tan Tao University, Ho Chi Minh City, Vietnam
3Pham Ngoc Thach University of Medicine, Department of Stem Cells, Ho Chi Minh City, Vietnam
4Japan National Institute of Infectious Disease, Tokyo, Japan
5Children's Hospital of Illinois, OSF Saint Francis Medical Center, Chicago, Illinois, USA
6Private Consultant, Tustin CA-USA
7Fribourg University Faculty of Science, Department of Medicine, Fribourg, Switzerland
- *Corresponding Author:
- Ciro Gargiulo
Human International Medical Center
Tan Tao University, Ho Chi Minh City, Vietnam
Tel: +8939778130
Fax: +89 38256724
E-mail: drciroisacco@gmail.coms
Received Date: October 26, 2016; Accepted Date: November 16, 2016; Published Date: September 19, 2016
Citation: Gargiulo C, Pham VH, Nguyen CDK, Vo TLH, Duy TH, et al. (2016) A Unique Case of Crossover Second Toe Syndrome Treated by Autologous Peripheral Blood Stem Cells. J Autoimmune Disord 3:1. doi: 10.21767/2471-8513.100028
Copyright: © 2016 Gargiulo C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Plantar plate tears, hammertoe, metatarsalgia, predislocation syndrome and metatarsophalangeal joint (MPJ) instability, all refer to what is commonly known as crossover second toe syndrome (CST). The CST, despite being widely present in the population, is a highly problematic condition that involves the entire structure of the foot and ankle including bones, muscles, tendons and joints. The CST is a form of degenerative condition associated with a progressive metabolic degenerative arthritis or arthrosis that leads to multiform forefoot deformities. Although the real underlying cause of the deformity is multifactorial, only some of the leading factors have been scientifically clarified, which make the prognosis quite problematic as the procedure needs to be proceeded on different levels and plans just to achieve an acceptable outcome, due to bone deformities, tendinopathies and neuropathies. Anatomically and pathologically, this condition is the result of the aging process, gradual deprivation of bone strength and a chronic inflammatory state induced by prolonged divergent and asymmetric mechanical forces of muscles and tendons. A strong pull of the flexor tendon medially and/or the attenuation of the lateral collateral ligaments of the second MPJ complex with valgus tendency related to a dorsal pull of the long and short extensor tendons without opposition from the plantar plate will result in a hammertoe deformity with dorsal contracture or dislocation of the toe at the MPJ. It has also been found that a long metatarsal together with prolonged periods of high peak pressures during walking are associated with the deformity and tears at the site of the plantar soft tissue. An adjunctive concern is caused by the hypermobility of the first ray linked with elevated pressures from the plantar to the second metatarsal head region. The direct pressure together with adducts of the hallux may cause dorsal displacement of the second toe. A case of a 56- year-old woman was presented to us with multiple joint osteo-arthritis and painful swelling on shoulders, bilateral knees, lower back, and ankles with a visible bilateral crossover second toe condition. An MRI and X-ray were performed, objectified a multiple osteoarthritis and grade 4 dual crossover second toe syndrome with deformity associated with hallux valgus, hallux rigidus, and neuroma of the third intermetatarsal space with metatarsus subluxation. The patient received a treatment of autologous PB-SCs infusion during a period of 3 weeks; the results showed a complete recovery of crossover second toe condition on both left and right foot.
Keywords
Crossover second toe syndrome; Peripheral blood stem cells; Telomere measurement; Rt-PCR
Introduction
The term “second crossover toe” (SCT) was firstly introduced by Coughlin in 1987 to describe a multi-plane deformity at the MPJ [1,2]. Anatomically and mechanically, the SCT deformity is a result of the instability of the whole foot-ankle structure. Here the defection of MPJ involves feebleness resulting from hallux abducto-valgus deformity and the gastrocnemius equinus. The MPJ disability may often be associated with a subluxation and/or dislocation of the dorsal and medial direction that may lead to a definitive plantar plate rupture and collateral ligament damage [2,3].
Eventually, the disorder causes a domino succession of events where each single component of the structure starts to fall apart. As lateral collateral ligament collapses, it leads to a medial deviation of the second toe and 3 of the plantar plates and the flexor tendon attachments become medially displaced. A neuroma may arise within the second intermetatarsal space as a consequence of the long term deterioration process, thus gradually and steadily, the whole structures of the 2nd MTP joint destabilize and collapse under the presence of chronic inflammation and trauma [1-5]. The end consequence is the growth of combined opposite-eccentric forces that tend to generate extra-additional medial displacement, with overwhelming pulling forces from extensor tendons [5-7].
The plantar plate is the second structure to cede. The insurgence of a weight-bearing distortion switches the proximal phalanx dorsally, as a consequence, there is an increased amount of resistance forces, deriving from both plantar plates and the intrinsic flexors (interossei and lumbricles), that drive the proximal phalanx back into a more resting position at the MTP joint. Hyperextension forces on the proximal phalanx play a crucial role on either stretching or weakening the plate, leading to a broader instability that ends up in a dorsomedial subluxation of the proximal phalanx on the metatarsal head [5-7].
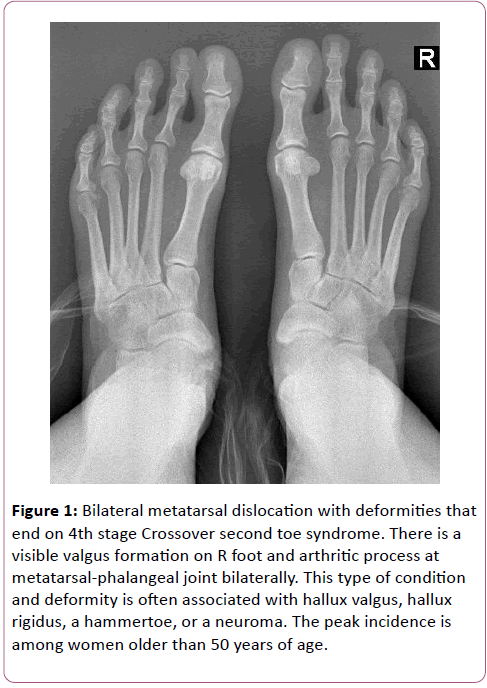
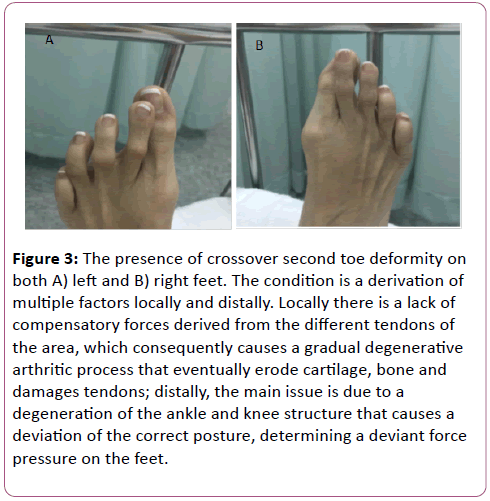
The on-going arthritic process and changes associated with systemic changes from rheumatoid arthritis and the inflammatory arthritis are certainly the most subtle influential factors that lead to a definitive degeneration of the tissues and components [3]. In relation to the current case of the 56-yearold woman presented with multiple joint osteoarthritis with painful and swelling on shoulders, bilateral knees, lower back and ankles with a visible bilateral crossover second toe condition (Figures 1-3), as far as we know, this is the first case of successful treatment of crossover second toe deformity by autologous PBSCs infusion within a period of just 21 days.
Figure 1: Bilateral metatarsal dislocation with deformities that end on 4th stage Crossover second toe syndrome. There is a visible valgus formation on R foot and arthritic process at metatarsal-phalangeal joint bilaterally. This type of condition and deformity is often associated with hallux valgus, hallux rigidus, a hammertoe, or a neuroma. The peak incidence is among women older than 50 years of age.
Figure 3: The presence of crossover second toe deformity on both A) left and B) right feet. The condition is a derivation of multiple factors locally and distally. Locally there is a lack of compensatory forces derived from the different tendons of the area, which consequently causes a gradual degenerative arthritic process that eventually erode cartilage, bone and damages tendons; distally, the main issue is due to a degeneration of the ankle and knee structure that causes a deviation of the correct posture, determining a deviant force pressure on the feet.
Case Presentation
The 56-year-old female displayed multiple site deforming osteo-arthritis. Six months prior to the visit she had received a complete bilateral knee prosthesis replacement. The patient was considerably overweight. The joint damages were visible on both ankles and feet with a bilateral second toe crossover condition. On physical examination, the supportive ligaments were noticeably weak, lead to failure of the joint and destabilization of the toe. Severe pain on both ankles and knees worsen during walking, the patient needed external-supports for moving around; the area of knees and ankles showed signs of swelling and tenderness, lower limb muscle atrophy with contracture was noticeable, deformities were present on both feet. The injured ankles’ active and passive range of motion were evaluated and compared with the contralateral movements, flexion, extension and rotation were assessed. During the assessment, the specificity of pain, including quality,radiation, timing, and aggravating factors were evaluated as well. In addition, the patient also pointed out the most painful area and indicated where the pain radiates from during walking.
Additional conditions and symptoms include fatigue, sleeping issues, nocturia, constipation, gastro-esophageal reflux (GERD), chronic urinary tract infection and weight gain.
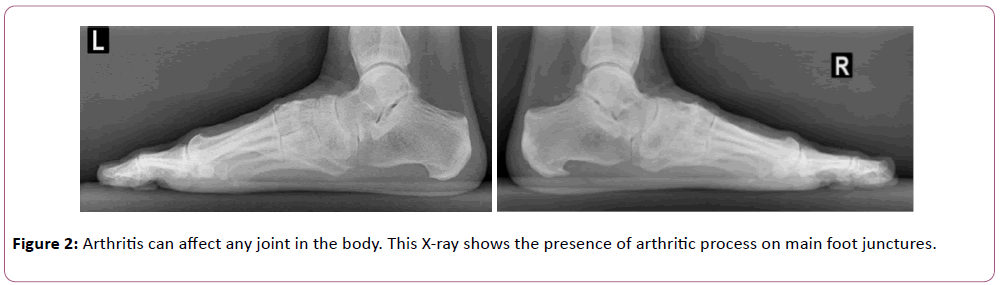
X-rays were performed and reified a grade 3/4 dual crossover second toe syndrome with a deformity associated with pronounced hallux valgus on the right side and, hallux rigidus on both right and left sides (Figure 1), and bilateral neuroma of the 3rd intermetatarsal space with metatarsus sub-luxation. The arthritic process was assessed on phalanges on both feet (Figure 2).
She was under prescribed medication as follows: Arthrotec (a combination of diclofenac and misoprostol), nonsteroidal antiinflammatory drugs (NSAIDs) to reduce pain and inflammation. Against the advice of her rheumatologist, she had recently discontinued taking prednisone due to significant side effects.
Imaging and Lab Tests
Clinical examinations performed in her hometown (MRI-X-ray) were sufficient for an accurate diagnosis; however additional laboratory tests were also performed:
Normal CBC count: Lipid and Liver profile: high Cholesterol 6.27 mM/L (normal range 3.37-5.18 mM/L);
Hormone profile: Estradiol high 53.26 pg/ ml (normal range post menop. 0-50), low Testosterone
2.64 ng/dl (normal range female 20-120 ng/dl), low IGF ≤ 25 ng/ml (normal range >40 to 50-250 ng/ml), low Vitamin D 11 ng/ml (normal range 50-150 ng/ml);
Immunity and Inflammation: TNFalpha high 10.6 pg/ml (normal range <8), Il 6 high 7.8 pg/ml (normal range <7).
Telomere analysis by RT-PCR CFX 96 (Biorad) has been performed at that time and the results showed normal activity of telomerase and long telomere inside cells: 12.5 Kb/ chromosome and 287.5 Kb/cells that increased after the treatment to 16.3 Kb and 376.8 (normal range 1.70 to 24.83 kb).
Treatment
An understanding of the subtle causes and annexed condition is an essential point to prevent further occurrences and exacerbations. While the endogenous inflammatory response is essential for the first step of the healing process, the control of its intensity, duration and pain is the goal of the initial phase of a specialist’s therapy. Conventional management of these issues is mainly based on the management of inflammatory processes and the first-line therapies include rests, corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs) with immobilizing splint [8-10].
Surgical intervention though considered effective and beneficial in nearly all cases [11], is the only solution left in those cases that do not respond well to more conservative management [12,13]. In the present case, the procedure presented some innovative aspects as it combined autologous PB-SCs together with plaster immobilization in association with active movements and a low glycaemic index diet as recommended in several edited studies [14,15]. The eligible patient was a 56 year old woman who has chosen stem cell therapy rather than conventional treatments (for reasons unrelated to the study), so it was possible to assess the association between changes in lifestyle and changes in telomere length without potentially confounding treatments. There were no specific inclusion criteria. The protocol for this study was approved by the TTU institutional review board. The patient had also provided a written informed consent.
Interventions
The patient underwent basic lifestyle intervention and a course of 15 injections of autologous PB-SCs, 1 injection per time, isolated and put in a serum-free cell culture medium in a culture-flask and positioned in a cell-incubator in our facility. Injections were performed using a micro-needle (JBP Japan), bilaterally and locally under medial malleoli, on Tibialis Anterior tendon, on Extensor Allucis longus and brevis, on 1st interosseus and on the insertion of Tibialis Posterior tendon. The patient received a course of supportive medication to enhance and promote mobilization of stem cells from bone marrow niches into circulatory system (Table 1). A physician and two nurses were on site during the procedures.
| MEDICINE | TIME | Ml |
|---|---|---|
| Vit B (Cenexi SAS France) | 5 | 2 |
| Vitamin D (HauptPharmaLivron France) | 4 | 1 |
| Hemax 4.000 I.U. (Biosidus SA Argenetina) | 3 | 2 |
| Vit B (Cenexi SAS France) | 2 | 5 |
| 15 | 10 | |
| GF2 (Laenex Lab. Japan) | 20 | 2 |
| GF1 (Lucchini Lab Swiss) | 1 | 2 |
| Hepatin (BTO Pharma.co. LTD Korea) | 1 | 5 |
| Hydrocortisone (Hsinchu Taiwan) | 1 | 2 |
| Vitamin C (Cenexi SAS France) | 7 | 5ml |
| GH implant | 1 | 8mg |
| Vit K (Rotexmedica Germany) | 4 | 10mg/1ml |
| Testosterone (Subcutaneous) | 1 | 100 mg |
Table 1: Supportive Medication.
After the first 6 months, another appointment is required and then continued twice a month for the duration of the study.
Peripheral blood mononuclear cells 35 ml blood was drawn from the participant into heparin tubes at baseline. The samples were anonymized so that laboratory technicians were unaware of the treatment group and collection time. PB-SCs were isolated within 1 hour with Ficollgradient (Ficoll-Paque PLUS, GE Healthcare, Pittsburgh, PA, USA) with ratio 1:2 (1 portion Ficoll, 2 portions blood). Viable PB-SCs were counted with the Trypan blue exclusion method (0.4% Trypan blue stain, Invitrogen, Grand Island, NY, USA) of 10/ml. Primary PB-SCs were cultured in 25-T flasks (Nunc-thermo scientific USA) with 5 ml SFM medium (Gibco Technologies USA) and incubated at 37°C-05% CO2 for 48 hours. PB-SCs (attached ones) were harvested by using 2 ml trypsin-EDTA and collected in 2 ml patient’s serum. Viable cells were counted using the Trypan blue exclusion method to obtain 10 cells/ml. After centrifugation at 5024 g in a refrigerated microcentrifuge (Silfradent, Bologna, Italy) at 4°C for 15 minutes, cells/pellets at the bottom was aspirated off.
Telomere length measurement by quantitative PCR
Real-time telomere quantitative PCR (qPCR) was used for the telomere length measurements. The method is well established and has been shown to be a reliable process to measure the telomere length in previous scientific studies and in basic researches [16]. Lymphocytes were collected from fresh blood by venepuncture into vacationer blood tubes (Silfradentheparine). The blood was diluted blood 1:1 with HBSS and gently invert to mix Overlay diluted blood onto 1/3 volume of Ficoll-Paque and centrifuged 400 g for 30 minutes at 20°C. Lymphocyte layers were moved to a fresh tube using a Pasteur pipette and diluted with 3X volume HBSS at room temperature. The entire solution was then centrifuged at 180 g for 10 minutes. Once supernatant was discarded the cell pellets were re-suspended in HBSS. Cell counts and viability tests were performed by using haemocytometer and trypan blue. The realtime qPCR method described by O’Callaghan and Fenech was used based on the Cawthon procedure for relative measurement of telomere length (TL) with a modification that considered the use of an oligomer standard to quantify a TL. Power SYBR I mastermix (Applied Biosystems, #4367396). Contained AmpliTaq Gold DNA polymerase, dNTPs, SYBR I Green Dye, opitimised buffers and passive reference dye (ROX). For this study, the β-globin gene (hgb) was used as the single copy reference. Real time kinetic quantitative PCR determines the fractional cycle (Ct) number at which the well’s accumulating fluorescence crosses a set threshold of 40 that is several standard deviations above baseline fluorescence. A standard curve is established by dilution of known quantities of a synthesized 84 mer oligonucleotide containing only TTAGGG repeats. The number of repeats in each standard is calculated using standard techniques, the oligomer standard is 84 bp in length (TTAGGG repeated 14 times), with a molecular weight (MW) of 26667.2, the weight of telomere standard is: 2.6667 × 104/6.02 × 1023=0.44 × 10-19 g. The highest concentration standard (TEL STD A) has 60 pg of telomere oligomer (60 × 10-12 g) per reaction, thus there are 60 × 10-12/0.44 × 10-19=1.36 × 109 molecules of oligomer in TEL STD A. The quantity of telomere sequence in TEL STD A is calculated based on the formula: 1.36 × 109 × 84 (oligomer length) =1.18 × 108 kb of telomere sequence in TEL STD A. A standard curve has been obtained by a calculation based on aTLqPCR assay on serial dilutions of TEL STD A (10-1 [1.18 × 108] through to 10-6 [1.18 × 103] dilution). In order to keep a constant 20 ng of total DNA per reaction tube, plasmid DNA (pBR322) was supplemented to each standard. The information of telomeric sequence per sample in kb was measured by using the standard curve.
Discussion
Though some disagreement regarding the true etiology of crossover second toe syndrome does exist, the general common evaluation is to describe it as a gradual degenerative condition where the foot structure tends to deform under steady dynamic antithetic and non-compensatory forces, which belong to the structure itself.
Haddad was the first who proposed a staging process for this syndrome, starting from synovitis and mild medial deviation at metatarsal joint, progressing to dorsomedial deviation (subluxation) at the metatarsal joint, staging to the overlapping of the Hallux and complete dislocation at the metatarsal joint synovitis. The entire process is accompanied by a constant inflammatory condition that surrounds the tendon sheaths, fascia plantaris and nerves and is associated to a bone degenerative condition known as osteoarthritis and rheumatoid arthritis; symptoms in the majority of cases are controlled by use of anti-inflammatory therapies, such as oral NSAID or peritendinous corticosteroid injections and eventually surgical intervention [16]. However, in the case of mild-severe deformities, the option is soft tissue surgery procedure or a shortening osteotomy of the second metatarsal, the distal oblique metatarsal osteotomy, known as Weil osteotomy [17,18].
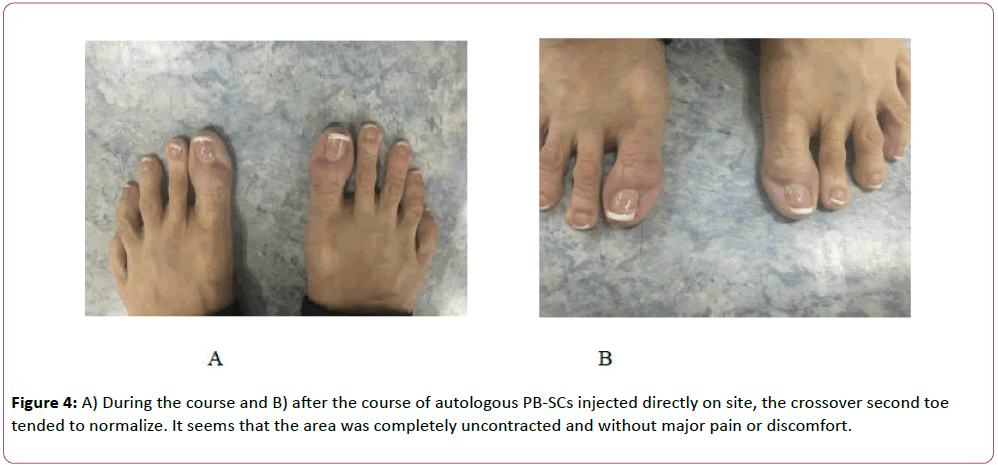
Here, we describe an autologous PB-SC–based therapy for SCT syndrome (Figure 4). Transplantation of hPB-SCs, which include both pluripotent and multipotent stem cells such as neural stem cells, mesenchymal stem cells, hematopoietic stem cells, embryonic like stem cells and progenitor NK cells in clinical application, have been the matter of our group’s recent research and publication [19,20].
However, the current case is a very unique case where this condition has been adjusted through e-cycles of autologous PBSCs micro injection either directly on pain sites or distally. Thanks to immune-modulatory properties, regenerative ability and anti-inflammatory effects of stem cells present in peripheral blood, the affected area eased, showing an improvement either on mobility or pain and therefore in tendon contractility. The idea behind these improvements in such a short time may be related to stem cells ability to trigger the repair process by homing in to the damaged part of the tissue and carrying out regeneration.
Stem cells’ main task is the renovation of lost tissues; in this case, newly osteoblasts and tenocytes replace the dead ones and their progenitors. The immediate phase after their introduction is their modulating activity within their microenvironment, by introducing other cell types. This enables the restoration of missing proteins and growth factors, to an otherwise deficient environment, which are responsible for cell proliferation, cytoprotection, and angiogenesis, thus, recovering the lost tissue functions [21].
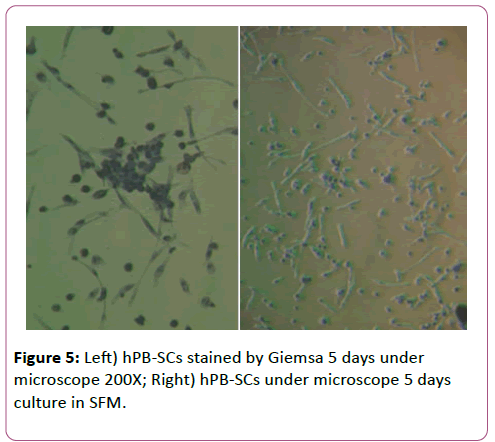
A further intriguing result that came out from this study is the increase of telomere length after the stem cell treatment. Telomere analysis by RT-PCR performed before treatment shows telomere length 12.5 Kb/single cell chromosome and 287.5 Kb/ totality cells. After the treatment an increase in telomere length is recorded, 16.3 Kb and 376.8 Kb (normal range 1.70 to 24.83 kb) respectively. As a well-accepted concept, telomere length diminishes with time leading to karyotype instability, senescence, apoptosis, or oncogenic transformation of somatic cells affecting life and expectancy [22,23]. Senescence per se is a process that has been associated with metabolic degenerative disorders, such as cardiovascular disease, diabetes, atherosclerosis, bone/cartilage degeneration and cancer. Thus, the major challenge is to determine the link between senescent cells and age-related tissue functionality, trying to point out a possible correlation in terms of cause-effect condition [24-26]. As proven in this case, the use of autologous hPB-SCs resulted in augmentation of telomere length has indicated visible beneficial effects on reassessing the crossover second toe condition, reducing pain and inflammation, and associated structure contractures (Figure 5).
Conclusions
This study is a part of a wider on-going project with hPB-SCs and degenerative condition and telomere. We understand that more data and evidence are needed to confirm and establish a more solid and valuable procedure.
Acknowledgment
All the listed authors have actively participated in groundwork, research and tuition of this current work.
Conflict of Interest
There is no conflict of interest to declare.
References
- DiDomenico LA, Rollandini J (2014) A closer look at tendon transfers for crossover hammertoe. Podiatry Today 27: 6.
- Thomas JL, Blitch EL, Chaney DM, Dinucci KA, Eickmeier K, et al. (2009) Diagnosis and treatment of forefoot disorders. Section 1: digital deformities. J Foot Ankle Surg 48:230-272.
- Nery C, Coughlin MJ, Baumfeld D, Raduana F, Szejnfeld MT (2015) Rev Bras Ortopedia 50:720–728.
- Karlock LG (2003) Second metatarsophalangeal joint fusion: A new technique for crossover hammertoe deformity: A preliminary report. J Foot Ankle Surg 42:178 –182.
- Coughlin MJ, Schenck RC, Shurnas PJ, Bloome DM (2002) Concurrent interdigital neuroma and MTP joint instability: long-term results of treatment. Foot Ankle Int 23:1018-1025.
- Kaz AJ, Coughlin MJ (2007) Crossover second toe: Demographics, etiology, and radiographic assessment. Foot Ankle Int 28:1223-1237.
- Deland JT, Sung IH (2000) The medial crossover toe: A cadaveric dissection. Foot and Ankle Int 21:375-378.
- Higgs PE, Mackinnon SE (1995) Repetitive motion injuries. Ann Rev Med 46:1-16.
- Hanlon DP, Luellen JR (1999) Intersection syndrome: A case report and review of the literature. J Emergency Med 17:969–971.
- Brinks A, Koes BW, Volkers AC, Verhaar JA (2010) Adverse effects of extra-articular corticosteroid injections: A systematic review. BMC Musculoskel Dis 11:206.
- Grundberg AB, Reagan DS (1985) Pathologic anatomy of the forearm: Intersection syndrome. J Hand Surg 10:299–302.
- Williams JG (1977) Surgical management of traumatic noninfective tenosynovitis of the wrist extensors. J Bone Joint Surg 59:408–410.
- Brunton LM, Wilgis EF (2010) A survey to determine current practice patterns in the surgical treatment of advanced thumb carpometacarpal osteoarthrosis. Hand 5:415–422.
- Mann JI, Hermansen K (2000) The Diabetes and Nutrition Study: Group of the European Association for the Study of Diabetes (EASD): Recommendations for the nutritional management of patients with diabetes mellitus. Eur J Clin Nutr. 54:353–355.
- Radulian G, Rusu E, Dragomir A, Posea M (2009) Metabolic effects of low glycaemic index diets. Nutr J 8:5
- Haddad SL, Sabbagh RC, Resch S, Myerson B, Myerson MS (1999) Results of flexor-to-extensor and extensor brevis tendon transfer for correction of the crossover second toe deformity. Foot Ankle Int 20:781-788.
- Myerson M, Jung HG (2005) The role of toe flexor-to-extensor transfer in correcting metatarsophalangeal joint instability of the second toe. Foot Ankle Int 26:675-679.
- Coughlin MJ, Mann RA (1993) Lesser toe deformities surgery of the Foot and Ankle. J Emergency Med 3: 72-85.
- Gargiulo C, Pham VH, Nguyen TH, Nguyen CDK, Phuc PV, et al. Isolation and characterization of multipotent and pluripotent stem cells from human peripheral blood. J fStem Cells Disc. 2015; 5:1-16.
- Fehlings MG, Vawda R (2011) Cellular treatments for spinal cord injury: the time is right for clinical trials. Neurotherapeutics 8:704–720.
- Goldman SA (2011) Progenitor cell-based treatment of the pediatric myelin disorders. Arch Neurology 68:848–856.
- Vaziri H, Dragowska W, Allsopp RC, Thomas TE, Harley CB (1994) Evidence for a mitotic clock in human hematopoietic stem cells: Loss of telomeric DNA with age. Proc Natl Acad Sci 91:9857.
- Shammas MA (2011) Telomeres, lifestyle, cancer, and aging. Curr Opin Clin Nutr Metab Care14: 28–34.
- Correia-Melo C, Hewitt G, Passos JF (2014) Telomeres, oxidative stress and inflammatory factors: partners in cellular senescence? Longevity Healthspan 3: 1.
- Gray JW, Collins C (2000) Genome changes and gene expression in human solid tumors. Carcinogenesis 21:443–452.
- Buxton J, Suderman M, Pappas JJ, Borghol N, McArdle W, et al.(2014) Human leukocyte telomere length is associated with DNA methylation levels in multiple subtelomeric and imprinted loci. Sci Rep 4:4954.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences